Where you live has a relationship to your odds of getting cancer and surviving cancer. Epidemiologists studying this link they see in the data have focused on so-called social determinants of health — poor access to transportation, for example, could make it harder for residents to see a doctor. Places lacking grocery stores with fresh food could mean worse nutrition for locals.
The worse outcomes for people from poorer, more stress-filled neighborhoods suggest that our physical and social spaces are somehow influencing our biology, said Brittany Jenkins-Lord, a molecular biologist at the Johns Hopkins Bloomberg School of Public Health. “Historically, this has been done in epidemiological ways, looking at risk factors and relating those to mortality or different kinds of outcomes,” she said. But exactly how something like a neighborhood might be influencing cancer biology is part of a growing field of study for scientists like her, Jenkins-Lord said. By examining things like tumor genetics, epigenetics, modifiers of gene expression, and other biological markers, they are starting to turn up intriguing results.
“Neighborhoods can impact expression of genes in this way and that could impact cancer outcomes,” Jenkins said. “Making that leap is intuitive but we haven’t had the data to do that. we haven’t had social determinant data and linking that to biology. That’s where we are right now as a field.”
Neighborhoods are like ecosystems in their complexity, with countless variables both small and large that could plausibly influence health and biology. For instance, the built environment, whether it has sidewalks or parks or polluting factories, and an area’s crime statistics could influence how easy it is for residents to exercise or spend time outdoors. “We think about working hours and how that impacts when people can see a doctor, diet and the food system,” said Hari Iyer, an epidemiologist at Rutgers Cancer Institute who studies neighborhoods. “It’s hard to collect every single thing. Neighborhood is a good proxy for all of these things.”
Scientists try to capture a rough, overall picture of the advantages or disadvantages that a neighborhood might provide through something called a “deprivation index.” These measure things like the average wealth and income, the education level, unemployment level, and occupations of the residents in a census tract. They also measure the housing quality in the census tract through things like the percentage of houses with incomplete plumbing or that are owner occupied.
In recent years, several studies have started to find that residents who live in neighborhoods with greater deprivation, based on one or more of these indexes, also seem to have concerning changes in the biology of their tumors. In the latest of these studies, published last month in JAMA Network Open, researchers at the University of Maryland and Virginia Commonwealth University looked at expression of certain stress-related genes in the prostate tumor cells of 218 men from Baltimore. Of the participants, 77% were Black, and the rest were white.
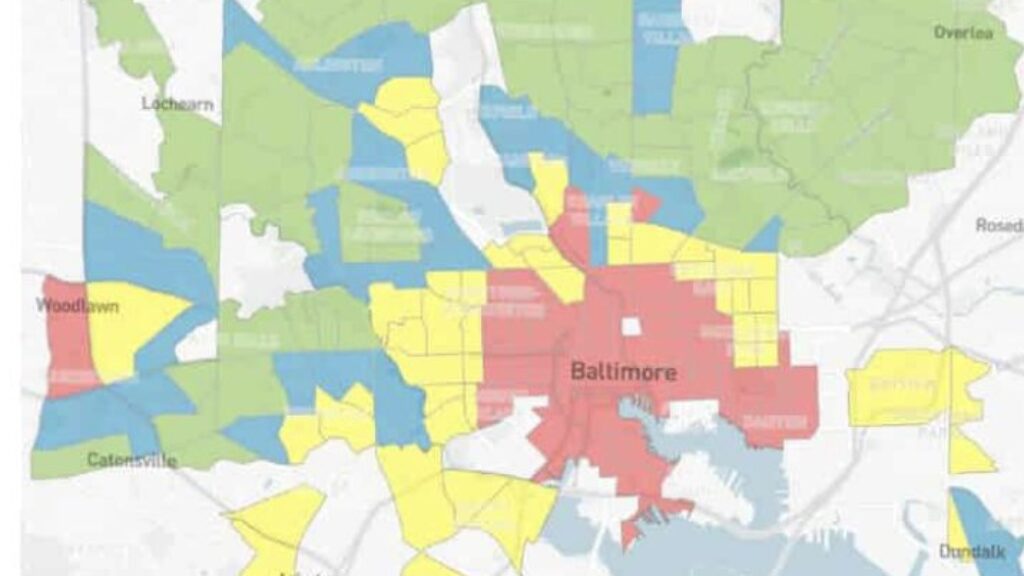
These researchers then looked at the participants’ neighborhoods based on three different indexes and whether they lived in a historically redlined area, a systematic and often race-based denial of investment in specific neighborhoods that became common in the 1930s. On all of these indexes, men who lived in areas of greater deprivation had slightly higher activation of stress and inflammation-related genes than those who lived in areas with less deprivation. The same was true for men who lived in a historically redlined area versus those who didn’t.
That means it’s possible living in worse-off neighborhoods could have had an effect on the prostate cancers of these men, said Kathryn Barry, a cancer epidemiologist at the University of Maryland School of Medicine and senior author on the paper. “The role of chronic stress due to living in disadvantaged areas, that may have downstream biological impacts like increased inflammation, and that could lead to increased risk of aggressive prostate cancer,” she said.
Other recent studies have uncovered similar signals hinting that the neighborhood you live in could be modifying the biology of cancer. Work from Johns Hopkins’ Jenkins-Lord published last year also found that higher neighborhood deprivation was linked to epigenetic changes and lowered expression of key genes in breast cancer. “Women from high deprivation areas had changes to two tumor suppressor genes. Lower expression of those gene suppressors is associated with worse survival, so much so that they can help predict who will survive and who will not,” she said.
Like other researchers, Jenkins-Lord found that African-American race correlated strongly with neighborhood deprivation. The contribution of ancestry could confound results from these neighborhood studies, Jenkins-Lord said. “Parsing out whether ancestry specific variants may be changing expression of tumor suppressors is difficult,” she said. “Is it environment? Is it genetics? Is it both and what is contributing more? We have more work to do that in that area.”
Or it could also be an indicator that some of the racial disparities in cancer outcomes, like the fact that Black men are more than twice as likely to die from prostate cancer and Black women are more than 40% more likely to die from breast cancer than white people, could be partially driven by neighborhood factors. “We’ll say Black people have worse outcomes because of their biology. Maybe. But maybe it’s not really their biology but race based on historical issues and societal structures, where we don’t have access to care,” said Robert Winn, the director of the Massey Cancer Center at Virginia Commonwealth University.
That the science is moving toward discovering signals related to neighborhoods within tumors is a strength, said Rutgers’ Iyer. “It’s not like you’re trying to make a claim from stress markers in blood,” he said. “No, it’s in the tumor, and it’s correlated with the environment. It’s helping us move closer to the argument like, hey, your stress might really impact your cancer and the progression of it.”
It’s also science that researchers hope will lead to informing community and neighborhood policies and public health interventions, Iyer said. Such research may show which neighborhood factors have the greatest impact on outcomes. In work that he’s done with the Veterans Affairs health care system, he’s found that racial disparities in prostate cancer were much smaller among veterans compared to those who were in the general population, even when they were from the same neighborhood. “To us, that was a pretty strong argument that with improving just access to care, you can do a lot,” Iyer said.
This work of establishing the relationship between social determinants of health and cancer outcomes is just beginning, said Massey’s Winn, who calls the emerging field the science of connecting the dots between “DNA and ZNA” or zip code neighborhood of association. “This is getting molecular responses to access to care, molecular response to where you live and the foods you have access to and missing the only bus that gets you to where you need to go,” Winn said. “It scratches the surface at this. We’re still in the bare-skinned sharp-knifed early stages.”